Continue Pathways Toward Increasing the Percentage of Nurses With a Baccalaureate Degree
Bridging the Gap: Seamless RN to BSN Degree Transitions
- Kathleen Carissimi, DNP, RN, CNS, CNE
- Jeri Burger, PhD, RN
- Article
- Figures/Tables
Abstract
The Institute of Medicine report, The Future of Nursing: Leading Change, Advancing Health, has recommended that the proportion of nurses with baccalaureate degrees be increased to 80% by 2020. As a response to this recommendation, leaders in nursing education have begun to explore strategies to implement seamless academic pathways to bridge the gap between diploma and associate-degree programs and baccalaureate-degree programs. These strategies are designed to eliminate curricular redundancy so programs will be attractive to registered nurses seeking this degree. In this article, the authors describe one State Action Coalition's initial steps to gain consensus for, and educate stakeholders about, a model designed to foster seamless educational progression pathways. The authors present their strategy for change, namely a competency-based model, discuss how their strategy unfolded, describe their project outcomes, address the project risks, and share lessons learned. They conclude that leaders in nursing education and service need to work collaboratively to support non-redundant pathways that lead to the baccalaureate degree.
Keywords: Future of Nursing: Campaign for Action, competency, competency-based curriculum, gap analysis, Institute of Medicine, nurse of the future models, Quality and Safety Education for Nurses (QSEN), seamless progression models, Campaign for Action, state action coalitions
The twentieth century, illness-focused curricular approaches to care delivery can no longer prepare nurses for the complexity of the current and emerging nursing practice environments. Nursing education is at a crossroads. The changing healthcare environment, including an aging population, increase in chronic conditions, equal access to care, reimbursement issues, and a shift from acute care to health promotion, is necessitating a transformation in nursing education (Cronenwett, 2011). The twentieth century, illness-focused curricular approaches to care delivery can no longer prepare nurses for the complexity of the current and emerging nursing practice environments (Ironside, 2004; Tanner, 2011).Reinforcing the need for change and opening the door for dialogue about how to best prepare the nurse of the future are landmark studies, such as Educating Nurses: a Call for Radical Transformation, and The Future of Nursing: Leading Change, Advancing Health (Benner, Sutphen, Leonard, & Day, 2010; Institute of Medicine, 2011).
The recent Institute of Medicine (IOM) report envisions the nursing profession as central to ensuring that the American public has access to high quality and cost-effective care (2011). The ability of the nursing profession to effectively respond to the future role of nurses is contingent upon its ability to respond to a second key message of the report. This essential message recommends that nurses achieve higher levels of education, through an educational system that promotes seamless academic progression, to facilitate nursing roles as leaders and equal partners in improving the healthcare system (Institute of Medicine, 2011).
With a 29% national benchmark deficit in BSN-prepared nurses, innovative and collaborative curricular interventions are crucial to achieve the Institute of Medicine 2011 vision. The 3.6 million nurses employed in the United States in a variety of healthcare settings are the intended recipients of this message (Campaign for Action, 2011). The IOM reported in 2011 that the percentage of nurses nationally with baccalaureate degrees in nursing was 50%, and has recommended that the percentage increase to 80% by 2020. A slight increase in the national percentage of employed nurses with baccalaureate degrees in nursing to 51% was noted by the Future of Nursing: Campaign for Action in 2013 (Campaign for Action, 2017). With a 29% national benchmark deficit in BSN-prepared nurses, innovative and collaborative curricular interventions are crucial to achieve the Institute of Medicine 2011 vision.
In this article, the authors describe the initial steps of one State Action Coalition to gain consensus and educate stakeholders about a model designed to foster seamless progression pathways. The authors first present their strategy for this change, a competency-based model. Next they discuss how the strategy unfolded, describe project outcomes, and address the project risks. They also share lessons learned and conclude by noting that leaders in nursing education and nursing service need to work collaboratively to support non-redundant pathways that lead to the baccalaureate degree.
Strategy for Change: Competency-Based Model
A competency-based curricular model to advance seamless academic progression is a dominant strategy emerging... A competency-based curricular model to advance seamless academic progression is a dominant strategy emerging from collaborative discussions about what, how, and where nursing students will learn to provide safe and effective care (American Association of Colleges of Nursing [AACN], 2012; Cronenwett, 2011; Spann, 2011; Sroczynski, Gravlin, Seymour Route, Hoffart, & Creelmam, 2011; Tanner, 2011). This strategy has been successful with several Campaign for Action state coalitions, including Oregon, Massachusetts, and Rhode Island, with the state of California as a leader in advancing the nurse of the future competencies (Sroczynski, 2013; Tanner, 2011). Although the definition of competency, and competency-based curriculum, are not consistently defined in the literature, a commonality of perspective does exist (Axley, 2008; Tilley, 2008) as described below.
The American Nurses Association defines competency as "an expected level of performance that results from an integration of knowledge, skills, abilities, and judgment" (2013, p. 3). Noonan (2012) has stated that a "competency model is a framework for organizing a collection of observable skills, behaviors, and attitudes that impact the quality of work that people do. It describes what people need to know and be able to do in order to execute on their responsibilities effectively" (p.1). Noonan (2012) has further suggested that competency gaps become inputs to align current performance to expected performance.
Competency models standardize outcomes, rather than curricular content... Competency models standardize outcomes, rather than curricular content, and are developed with input from both nursing education and nursing practice (Anema & McCoy, 2010; Pomatto, 2013). As such, competency models become effective strategies to align curricula and create seamless pathways from one degree to another, especially in transitions from diploma and associate degree programs to baccalaureate programs (Fauteux, 2013; Sroczynski, et al., 2011). Competency models ease the transition between diploma/associate degree programs to baccalaureate degree programs through initiatives, such as dual enrollment or dual admission to these two levels of programs or to a shared curriculum between the programs (Fauteux, 2013; Ohio Action Coalition, 2015).
The inclusion of practice partners in the development of the model ensures that competencies reflect the realities of the current practice environment. Curricula based on a competency model offer several advantages to students. Credits are more readily transferable in competency models because clear delineation of the competencies results from collaborative discussions between the degree programs (Close & Orlowski, 2015; Fauteux, 2013; Ohio Action Coalition, 2015). Seamless curricular strategies also increase the likelihood of completing the diploma/associate degree and the BSN degree in four years (Fauteux, 2013; Sroczynski, et al., 2011). Furthermore, competency models have potential to close the education-practice gap. The inclusion of practice partners in the development of the model ensures that competencies reflect the realities of the current practice environment (Sroczynski, et al., 2011). This education and practice collaboration is particularly important in developing competencies to achieve safety and quality initiatives (Berwick, 2011; Burns & Poster, 2008; Cronenwett, 2011; Tanner, 2011).
The Strategy Unfolds: Project Description
This section will explain the linkage between the Ohio Action Coalition Project to increase the number of baccalaureate-prepared nurses and first author's (Dr. Carissimi's) Doctor of Nursing Practice (DNP) capstone project. It will also describe the project's purpose and scope, outcomes, and risks, and share the lessons learned through this project.
The Ohio Action Coalition Project and Capstone Project Linkage
...a coalition includes leaders in nursing practice and nursing education, health providers, and legislators. The Future of Nursing: Campaign for Action is a national initiative funded by the Robert Wood Johnson Foundation, the American Association of Retired Persons (AARP), and the AARP Foundation to advance the 2011 IOM, Future of Nursing recommendations (Campaign for Action, 2011). The Campaign for Action (2011) has assisted 50 states, including Ohio, to form action coalitions. The Ohio Action Coalition (OAC) is led by representatives from the Ohio League for Nursing and the Ohio Hospital Association. Action coalitions are composed of a wide variety of stakeholders who are interested in advancing the profession of nursing; a coalition includes leaders in nursing practice and nursing education, health providers, and legislators. At the time of the IOM (2011) report, the percentage of BSN-prepared nurses in Ohio was 31% (Ohio Board of Nursing, 2011). The Ohio Action Coalition elected to focus its statewide project on the Institute of Medicine recommendation for increasing the number of baccalaureate-prepared nurses to 80% by 2020 through the use of a competency-based model as a seamless academic progression model (2011). The statewide project began in March 2013.The percentage of BSN-prepared nurses in Ohio, as of August, 2013, was reported to be 34% (Ohio Board of Nursing, August, 2013).
The formation and evolution of the OAC statewide project set the stage for the first author's capstone project. The first author applied for, and was appointed, as one of four co-chairs to the OAC work group, Increasing BSNs in the Workforce. At the time of this appointment, the first author also was in the process of completing a DNP. A degree requirement was completion of an evidence-based capstone project, focused on improving healthcare outcomes. The capstone project was based on the OAC statewide project. This involved assessing and tracking development and implementation of the statewide, competency-based model designed to increase the number of BSN-prepared nurses in the Ohio workforce. The decision to combine the role of work group co-chair for the OAC statewide project with the DNP capstone was approved by the three other work group co-chairs, Joy Bischoff, Le-Ann Harris, and Cindy Wilkins. Jane F. Mahowald, OAC co-leader, granted permission to use the OAC project as the first author's capstone project and Dr. Jeri Burger, co-author and capstone mentor, also approved the project.
Capstone Project: Purpose and Scope
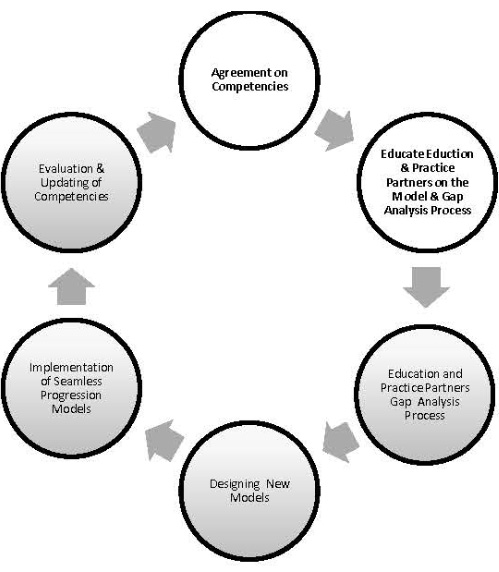
The scope of the capstone project, along with parallel activities as a work group co-chair for Increasing BSNs in the Workforce project, is best understood by examining the process steps used to develop the Ohio competency model. This cyclical process involved six steps: Step 1: agreement on competencies through adoption of a statewide competency model; Step 2: education of pre-licensure nursing programs, and the programs' clinical practice partners about the competency model; Step 3: completion of the gap analysis process; Step 4: designing new education models by addressing gaps; Step 5: implementing seamless progression models; and Step 6: evaluation and updating of competencies (Sroczynski, 2013). The first author's role and responsibilities for both the OAC work group and capstone project revolved around the first two steps of the process. A schematic of this process is illustrated in Figure 1.
The Increasing BSNs in the Workforce team was comprised of four work group co-chairs and approximately 50 volunteers from nursing education, nursing practice, and other healthcare sectors. Two nursing education and two nursing practice work group co-chairs were appointed following a formal application process. The role and responsibilities of the four work group co-chairs were to facilitate delivery of the first two steps of the competency model development process.
Initiation of step one of the process began with the work group co-chairs convening and directing a series of working meetings with volunteer members of the work group. The purpose of the meetings was to develop and gain consensus on the Ohio Competency Model. In conjunction with the other work group co-chairs, facilitated these working meetings. The second step of the cyclical process, education about the model, involved the author and other work group co-chairs serving as co-moderators for several statewide, regional sessions designed to educate practice and education stakeholders about the competency model and the gap analysis. The first author's participation in regional educational sessions was limited to the central and southwest Ohio sessions.
Figure 1: Competency Model Development Process
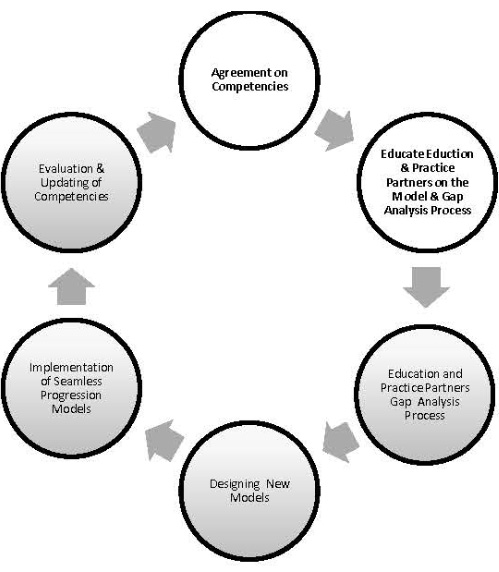
Adapted with permission from: Sroczynski, M. (2013). The competency or outcomes based curricular model: Recipe for success
The second step of the cyclical process involved participation by work group co-chairs in the development of a survey. This survey assessed the progress of nurse educators and practice partners in initiating the gap analysis process following their participation in the educational sessions. The survey results would then inform development of strategies for initiating the third step of the competency development process, engagement of partners in the gap analysis, Step three was implemented under the leadership of Carol Drennen, Project Director for the OAC's Future of Nursing State Implementation Program (SIP) grant. Analyzing and sharing survey results concluded the capstone project and the first author's active participation in the statewide project.
The Ohio Action Coalition nursing co-lead, Jane F. Mahowald, and the Center to Champion Nursing in America (CCNA) Nursing Expert/Consultant, Maureen Sroczynski, were also instrumental during these initial steps. Both individuals added clarity and direction to the intent of the Increasing BSNs in the Workforce initiative during model development and consensus, and served as co-moderators during the educational sessions and contributors to the post-education survey. Dr. Sroczynski also provided expertise and experience in developing and implementing competency models. Table 1 identifies key individuals and their roles in this Ohio, statewide project.
Capstone Project Outcomes
Outcome #1: Competency Model Development
The model was developed through input from work team co-chairs and members of the OAC work group. Increasing BSNs in the Workforce. The capstone project was designed to achieve three short-term outcomes: a) development and agreement on the Ohio Competency Model; b) education of pre-licensure nursing programs and their practice partners regarding the model; and, simultaneously, c) education about the gap analysis process. The first outcome, to develop a competency-based model through consensus of key stakeholders, was initiated in March 2013 and completed in February 2014. The model was developed through input from work team co-chairs and members of the OAC work group. Increasing BSNs in the Workforce. All members of this work team, including appointed co-chairs, volunteered to participate in this initiative. The majority of the members were nurses in various roles in education and/or practice settings. Examples of roles included staff nurses, Magnet® coordinators, clinical educators, nursing administrators, nursing education administrators, and faculty.
Table 1: Role of Key Individuals in the Ohio Action Coalition Statewide Project
| Name | Title | OAC Role |
| Joy Bischoff, MSN, RN | VP Patient Services, Chief Nursing Officer, Ohio Health, Marion General Hospital | Increasing BSNs Work Group- Co-Chair-Practice |
| Kathleen Carissimi, DNP, RN, MEd, CNS, CNE | Director RN to BSN Program, University of Cincinnati | Increasing BSNs Work Group- Co-Chair-Education |
| Carol Drennen, MSN, MS, RN | Project Director, SIP Grant | Project Director, SIP Grant |
| Le-Ann Harris, DNP, RN, NEA-BC | Director of Nursing, Critical Care & Trauma, | Increasing BSNs Work Group- Co-Chair-Practice |
| Jane F. Mahowald, MA, RN, ANEF | Executive Director, Ohio League for Nursing | Ohio Action Coalition, Nursing, Co-Lead |
| Maureen Sroczynski, DNP, RN | President/CEO | Consultant, Center to Champion Nursing |
| Cindy Wilkins, PhD, RN | Director & Chair of Nursing Programs, Muskingum University | Increasing BSNs Work Group- Co-Chair- Education |
The final Ohio Nurse Competency Model document consisted of the seven competency statements, competency definitions, and corresponding knowledge, skills, and attitudes (KSAs) for each competency. The model was derived from both the Quality and Safety Education for Nurses (QSEN) and Massachusetts Nurse of the Future (NOF-MA) models (Cronenwett et al., 2007; Massachusetts Department of Higher Education, 2010). Figure 2 depicts a schematic of the seven competencies: 1) patient-centered care; 2) leadership and professionalism; 3) evidence-based practice; 4) quality improvement and safety; 5) information and technology; 6) communication, teamwork, and collaboration; and 7) systems-based practice. Selected examples of competency statements for patient-centered care and communication, teamwork, and collaboration can be found in Table 2. Only a partial replication of the KSAs for each of these competencies is provided. The complete document for the Ohio Nurse Competency Model can be found on the OAC's web page under Historical Data (Ohio Action Coalition, 2014, May).
Figure 2: Ohio Nurse Competency Model
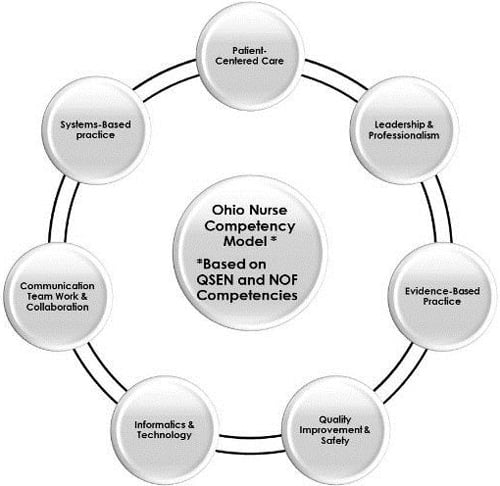
Brainstorming was used as a strategy for reaching consensus on the model. Brainstorming was used as a strategy for reaching consensus on the model. The agenda for the first meeting included formation of brain storming groups. Each group was composed of associate degree and diploma program faculty, baccalaureate degree faculty, and nursing practice representatives. The afternoon session used information from the morning sessions to group similar competencies into categories. This specific activity provided the co-chairs with information that laid the foundation for future meetings to define the Ohio model. The number of competencies in the final model highlights the desire to ensure that consensus reflected opinions of all involved stakeholders.
Table 2: Examples of Competency Statements for the Ohio Nurse Competency Model
| PATIENT-CENTERED CARE (QSEN) Definition: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient's preferences, values, and needs. | ||
| Knowledge Describe how diverse cultural, ethnic, and social backgrounds function as sources of patient, family, and community value. | Skills Provide patient-centered care with sensitivity and respect for the diversity of human experience. | Attitudes Seek learning opportunities with patients who represent all aspects of human diversity. |
| COMMUNICATION, TEAMWORK, & COLLABORATION (NOF-MA & QSEN) Definition: Interact, effectively, with patients and families and within nursing and inter-professional teams, to foster open communication, mutual respect, and shared decision-making, to achieve quality patient care and positive health outcomes, and to enhance patient satisfaction. | ||
| Knowledge Describe scopes of practice and roles of healthcare team members. Describe strategies for identifying and managing overlaps in team member roles and accountabilities. Recognize contributions of other individuals and groups in helping patient/family achieve health goals. | Skills Function competently within own scope of practice as a member of the healthcare team. Assume role of team member or leader based on the situation. Initiate requests for help when appropriate to situation. Clarify roles and accountabilities under conditions of potential overlap in team member functioning. | Attitudes Value the perspectives and expertise of all health team members. Respect the centrality of the patient/family as core members of any healthcare team. Respect the unique attributes that members bring to a team, including variations in professional orientations and accountabilities. |
Outcome #2: Educational Sessions
The second project outcome, education about the model, was facilitated through a series of five regional meetings held in spring 2014. The OAC hosted meetings in the northeast, northwest, central, southeast, and southwest regions of the state to maximize diffusion of the project. Major objectives of the meetings included; a) a description of the Ohio Nurse Competency Model, b) an explanation of how the model could facilitate an increase of BSNs in the Ohio workforce, and c) presentation of the gap analysis process. Each educational session included stakeholders from diploma, associate degree, and baccalaureate nursing education. The group also included nurse administrators or their designees from practice settings used for clinical experiences by nursing programs.
Outcome #3: The Gap Analysis Process
An expected outcome following the educational sessions was that pre-licensure nursing programs and their clinical practice partners would begin initial discussions to identify the gaps between the Ohio Nurse Competency Model and their current program curricula. These discussions also provided an excellent opportunity for educators and clinical partners to identify inconsistencies between program competencies and practice environment expectations. Consequently, an understanding of the term 'gap analysis' and the process of gap analysis was an integral component for participants to master during these educational sessions.
A gap analysis asks the questions where are you and where do you want to be? A gap analysis is the process of identifying the current state of a situation and determining needs to arrive at a future state (BusinessDictionary.com, n.d.). A gap analysis asks the questions where are you and where do you want to be? Sroczynski et al. (2011) reiterated that the purpose of a gap analysis is to compare the current state of nursing curricula to the desired state of the competency-based curriculum. The difference between current state and desired state is termed the gap.
Inclusion of clinical practice partners in the gap analysis ensured that the analysis captured the realities of the practice environment. The current state in this project was the nursing curricula of pre-licensure programs and the future state was the Ohio Nurse Competency Model. Comparison between the desired competencies of the Ohio Model and current status of nursing curricula revealed gaps between the current and desired state. This technique is an effective method to determine deficiencies of what is and what should be, in terms of knowledge and performance (Sroczynski et al., 2011). Inclusion of clinical practice partners in the gap analysis ensured that the analysis captured the realities of the practice environment.
A survey tool was developed by the OAC co-lead, the Increasing BSNs in the Workforce work group co-chairs, and the Center to Champion Nursing in America (CCNA) consultant. Approximately three months after the regional educational sessions, participants received the survey requesting a status report on progress with the gap analysis process. Survey results served as a tool to guide the next steps of the work group. The OAC Regional Meeting Follow-Up Survey was e-mailed to all meeting participants on September 2, 2014, with a request for completion by September 10, 2014. Completion of the survey was considered informed consent for this project.
The fact that regional stakeholders continued to educate and engage other educators and practice partners became a win-win for the work group. Of 147 e-mailed surveys, a total of 24 were returned for a 16.3 % return rate. Low participation levels hindered meaningful discussion of survey results. However, survey comments suggested that education and engagement about the Ohio Nurse Competency Model were continuing through discussion and collaboration within nursing programs and practice settings. Survey responses, such as "shared model with faculty," "discussed with two community colleges and one RN to BSN program," and "stimulated discussion with partnerships," demonstrated continued dissemination of the model following regional education sessions. The fact that regional stakeholders continued to educate and engage other educators and practice partners became a win-win for the work group.
Risks of the Project
The major risk for the capstone project was the unexpected delay in completing step one, development and consensus agreement on the competencies. This was the most crucial phase for the project as it was the foundation for the education about the competencies, their corresponding knowledge, skills, and attitudes, and the basis for the gap analysis. In July 2013, the Increasing BSNs in the Workforce group met and voted by consensus that the Ohio Action Coalition would adopt the Massachusetts Nurse of the Future model, unaware of the risk associated with this decision. However, the same intuitiveness that alerts a nurse when all is not right with a patient, led the co-chairs to suspect that true consensus on the model had not yet been achieved.
...a major impediment to consensus was the failure to include the QSEN competencies in the Ohio model. The CCNA consultant, the OAC leadership, and the work group co-chairs began an assessment of the situation. They found that a major impediment to consensus was the failure to include the QSEN competencies in the Ohio model. The QSEN Institute is located at the Frances Payne Bolton School of Nursing, Case Western Reserve University in Cleveland, Ohio. Consequently, the QSEN model had become very entrenched in both the nursing education and practice settings in Ohio. Lengthy teleconferences were held with work group members and QSEN stakeholders to identify possible solutions. The final Ohio Nurse Competency Model merged the Massachusetts Nurse of the Future and QSEN models. The Ohio Nurse Competency Model was adopted in February 2014.
Key stakeholders had to be willing to commit the time to be educated and to accurately complete the gap analysis tool for each of the seven competencies. Volunteers served as key leaders of the initiative. Consequently, a potential risk for membership attrition existed. Although there were several inter-agency education and practice exchanges among the members of the Increasing BSNs in the Workforce group, one constant was the consistent commitment of the project co-chairs, the OAC nursing co-lead, and the CCNA consultant during the tenure of the project. Key stakeholders had to be willing to commit the time to be educated and to accurately complete the gap analysis tool for each of the seven competencies. Although the capstone project only addressed the first two steps of the process, the time intensity and subjectivity associated with the gap analysis tool were also important risk factors to consider as the state project progressed.
Another risk was the initial idea of making the Ohio Nurse Competency Model a mandatory model for nursing education. Intricacies of how to mandate the model were never discussed. The decision to decrease risk by moving from a mandatory to volunteer model was based on Roger's Diffusion of Innovation Theory. This theory describes the process of adopting a new idea. For the project, emphasis was on the adopter categories of 'innovators,' early adopters, early majority, late majority, and laggards' (Kaminski, 2011). Rogers stressed that as the "early innovators spread the word ... more and more people become open to the idea" (Kaminski, 2011, para. 1). An additional risk was the expectation that increased participation by education-practice cohorts in the gap analysis process, would occur as a result of regional volunteers spreading the word.
A low return rate of 16.3% on the OAC Regional Meeting Follow-Up Survey can also be viewed as a potential risk related to evaluation of project outcomes. However, information gained from the survey did assist with decisions about next steps to facilitate the gap analysis process among education and practice partners.
Seamless Academic Pathways: Lessons Learned
The capstone project ran parallel with the OAC's work group project to increase the number of BSN-prepared nurses in the Ohio workforce. Outcomes of the capstone project were achieved. The statewide Ohio Nurse Competency Model and its corresponding competency statements were adopted and regionally disseminated in educational sessions. Survey results were analyzed and reported to the work group and the OAC Steering Committee.
A major lesson learned was the difficulty advancing such a large scale project with a work group comprised of volunteers. A major lesson learned was the difficulty advancing such a large scale project with a work group comprised of volunteers. Work group co-chairs and members maintained full or part time jobs beyond their work group roles. Additionally, co-chairs and members were located in different parts of the state. Thus, because there was often a gap of several weeks between meetings, there was a need to regroup and gather momentum at the start of each work session. Both 'lessons learned' contributed to a timespan of almost a year to complete the development and consensus phase. The unforeseen difficulty in hiring a project director also may have added to project delay due to lack of a single coordinating individual.
We also learned that, while both education and practice co-chairs and members of the work group were all committed to the common goals to develop and reach consensus on a competency model, achieving that goal was a very time-consuming process. Finally, we learned to never ignore the "meeting after the meeting." Frequently that is where issues blocking consensus were actually addressed.
Conclusion
The first two steps of the competency model development process were just the beginning of efforts to engage and educate academic and practice partners about using the Ohio Nurse Competency Model to facilitate development of seamless academic progression models. It would be premature to imply any correlation between the advent of the Ohio competency model and the increased percentages of BSN-prepared nurse in the Ohio workforce. However, the Ohio Board of Nursing, in 2015, did report that 36% of licensed registered nurses in the Ohio workforce were BSN-prepared, an increase of five percent since 2015.
Progress in achieving the IOM (2011) recommendation to increase the number of BSN-prepared nurses to 80% by 2020 has resulted from collaborative efforts of state action coalitions, such as the Ohio Action Coalition, to create models that facilitate seamless transitions from a diploma or associate degree program to baccalaureate programs. The number of RN to BSN graduates increased from 34.5% in 2011 to 43% in 2014 (AACN, 2015). However, the number of BSN-prepared nurses nationally had only marginally increased to 51% by 2014 (Campaign for Action, 2015).
Commitment of leaders in the nursing profession to increase innovative educational opportunities that support academic pathways toward the baccalaureate degree must continue if the 2020 goal is to be realized. Commitment of leaders in the nursing profession to increase innovative educational opportunities that support academic pathways toward the baccalaureate degree must continue if the 2020 goal is to be realized. The Ohio Action Coalition competency model to create efficient and effective pathways to obtain the BSN degree demonstrates one such collaborative strategy that can, seamlessly, assist registered nurses to bridge the gap in the transition between degrees. Leaders in nursing education and nursing service need to continue working collaboratively to increase pathways that support efficient and effective movement toward obtaining BSN degrees.
Authors
Kathleen Carissimi, DNP, RN, CNS, CNE
Email: Kathleen.carissimi@uc.edu
Dr. Carissimi holds a DNP degree from the University of Southern Indiana University in Organizational and Systems Leadership. Her current experience as the Director of an online RN to BSN program and her previous experiences as a faculty member, Assistant Director of a diploma program, and Dean of an associate degree program have provided her with a unique perspective into the curricular needs of registered nurses returning for the baccalaureate in nursing degree. Dr. Carissimi is a member of the Ohio Action Coalition (OAC) Steering Committee and is one of four co-leads for the OAC's work group to increase the number of BSN-prepared nurses in the Ohio workforce. She is also holds National League for nursing certification as a nurse educator (CNE).
Jeri Burger, PhD, RN
Email: Jlburger2@usi.edu
Dr. Jeri L Burger holds a BA degree in nursing from Augustan College, an MS degree in nursing with a focus on nursing education from the University of Minnesota, and a PhD in nursing from Saint Louis University. She has spent much of her career in nursing education with an emphasis on undergraduate nursing education. She has taught in BSN programs with traditional BSN students, second degree BSN students, and RN-BSN students. She also has extensive experience with face-to-face and online course delivery. She is currently Chair of the RN Completion Program at the University of Southern Indiana.
References
American Association of Colleges of Nursing. (2012). Joint statement on academic progression for nursing students and graduates [Position statement]. Retrieved from http://www.aacn.nche.edu/aacn-publications/position/joint-statement-academic-progression
American Association of Colleges of Nursing. (2015). Degree Completion Programs for Registered Nurses: RN to Master's Degree and RN to Baccalaureate Programs. Retrieved from http://www.aacn.nche.edu/media-relations/fact-sheets/degree-completion-programs.
American Nurses Association. (2013, August). Competency model. Retrieved from https://learn.ana-nursingknowledge.org/template/ana/publications_pdf/leadershipInstitute_competency_model_brochure.pdf
Anema, M. G., & McCoy, J. (2010). Competency-based nursing education: Guide to achieving outstanding learner outcomes. New York, NY: Springer.
Axley, L. (2008). Competency: A concept analysis. Nursing Forum, 43(4), 214-222.
Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. Hoboken, NJ: John Wiley & Sons, Inc.
Berwick, D. (2011). Preparing nurses for participation in and leadership of continual improvement. In The future of nursing: Leading change, advancing health (pp. 494-504). Washington, DC: National Academies Press. Retrieved from http://www.nap.edu/catalog/12956.html
Burns, P., & Poster, E. (2008). Competency development in new registered nurse graduates: Closing the gap between education and practice. The Journal of Nursing Education, 39(2), 67-73.
BusinessDictionary.com. (n.d.). Gap analysis. Retrieved from http://www.businessdictionary.com/definition/gap-analysis.html
Campaign for Action. (2017). Future of nursing: Campaign for action. Retrieved from http://campaignforaction.org/
Campaign for Action. 2015. Campaign progress: Dashboard indicators. Retrieved from https://campaignforaction.org/resource/dashboard-indicators/
Close, L., & Orlowski, C. (2015). Advancing associate degree in nursing-to-baccalaureate degree in nursing academic progression: The California collaborative model for nursing education. Journal of Nursing Education, 54(12), 683-688. Doi: 10.3928/01484834-20151110-04.
Cronenwett, L., Sherwood, G., Barnsteiner J., Disch, J., Johnson, J., Mitchell, P., Sullivan, D., Warren, J. (2007). Quality and safety education for nurses. Nursing Outlook, 55(4)122-131. DOI: http://dx.doi.org/10.1016/j.outlook.2007.02.006
Cronenwett, L. (Ed.). (2011). The future of nursing education. The future of nursing: Leading change, advancing health (pp. 477-482). Washington, DC: The National Academies Press. Retrieved from http://www.nap.edu/catalog/12956.html
Fauteux, N. (2013). The case for academic progression: Why nurses should advance their education and the strategies that make this feasible. Charting Nursing's Future, 1-8. Retrieved from http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2013/rwjf407597
Institute of Medicine. (2011). The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press. doi:10.17226/12956.
Ironside, P. (2004). "Covering content" and teaching thinking: Deconstructing the additive curriculum. Journal of Nursing Education, 43(1), 5-12. Retrieved from https://oied.ncsu.edu/faculty/wp-content/uploads/2015/03/PDF/Covering-Content-and-Teaching-Thinking.pdf?boxtype=pdf&g=false&s=false&s2=false&r=wide
Kaminski, J. (2011). Diffusion of innovation theory. Canadian Journal of Nursing Informatics, 6(2). Retrieved from http://cjni.net/journal/?p=1444
Massachusetts Department of Higher Education. (2010). Creativity and connections: Building the framework for the future of nursing education and practice: Massachusetts Department of Higher Education nursing initiative nurse of the future: Nursing core competencies©. Retrieved from http://www.mass.edu/currentinit/documents/NursingCoreCompetencies.pdf
Noonan, M. (2012). Competency Models – What are they anyhow and what's the big deal?. St. Charles Consulting Group, LLC, 27, 1-2. Retrieved from http://www.stccg.com/competency-models-what-are-they/
Ohio Action Coalition. (2014, May). Historical data: Final Ohio nurse competency model. Retrieved from https://c.ymcdn.com/sites/oln.site-ym.com/resource/resmgr/ohio_action_coalition/FINAL_Ohio_Nurse_Competency_.pdf
Ohio Action Coalition. (2015, October). OPENing doors: Ohio pathways for education in nursing: A toolkit for developing nursing education progression models through a competency based curriculum. Retrieved from http://www.ohioleaguefornursing.org/resource/resmgr/ohio_action_coalition/SIP_2_Toolkit_for_Model_Deve.pdf
Ohio Board of Nursing. (2011). Ohio workforce survey data summary. Retrieved from http://www.nursing.ohio.gov/PDFS/workforce/1.3.1Workforce-Memo.pdf
Ohio Board of Nursing. (2013). 2013 RN: Ohio workforce data summary report. Columbus, OH: Ohio Board of Nursing. Retrieved from http://www.nursing.ohio.gov/PDFS/workforce/RN_Workforce_2013.pdf
Ohio Board of Nursing. (2015). 2015 RN: Ohio workforce data summary report. Columbus OH: Retrieved from http://www.nursing.ohio.gov/PDFS/Workforce/2015RN/RN%20Workforce%202015%20FINALREV.pdf
Pomatto, M. C. (2013). Models of academic progression. Retrieved from http://www.kansasactioncoalition.com/uploads/1/6/5/8/16583712/models_of_academic_progression-_october_2013.pdf
Spann, J. (2011). Implementing the Institute of Medicine future of nursing report-Part I: How to dramatically increase the formal education of America's nursing workforce by 2020. Charting Nursing's Future, 1-8. Retrieved from http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2011/rwjf70968
Sroczynski, M., Gravlin, G., Seymour Route, P., Hoffart, N., & Creelmam, P. (2011). Creativity and connections: The future of nursing education and practice: The Massachusetts initiative. Journal of Professional Nursing (online), 27(6), 64-70. Retrieved from http://www.mass.edu/currentinit/documents/Nursing/NOFArticle.pdf
Sroczynski, M. (2013). The competency or outcomes based curricular model: Recipe for success. Consultant, Center to Champion Nursing in America. Retrieved from https://campaignforaction.org/resource/competency-model-webinar-part-1/
Tanner, C. (2011). Transforming pre-licensure nursing education: Preparing the new nurse to meet emerging health care needs. In The future of nursing: Leading change, advancing health. (pp. 536-550). Washington, DC: The National Academies Press. Retrieved from http://www.nap.edu/catalog/12956.html
Tilley, D. (2008). Competency in nursing: A concept analysis. The Journal of Continuing Education in Nursing, 39(2), 58-64.
Figure 1: Competency Model Development Process
Adapted with permission from: Sroczynski, M. (2013). The competency or outcomes based curricular model: Recipe for success
Table 1: Role of Key Individuals in the Ohio Action Coalition Statewide Project
| Name | Title | OAC Role |
| Joy Bischoff, MSN, RN | VP Patient Services, Chief Nursing Officer, Ohio Health, Marion General Hospital | Increasing BSNs Work Group- Co-Chair-Practice |
| Kathleen Carissimi, DNP, RN, MEd, CNS, CNE | Director RN to BSN Program, University of Cincinnati | Increasing BSNs Work Group- Co-Chair-Education |
| Carol Drennen, MSN, MS, RN | Project Director, SIP Grant | Project Director, SIP Grant |
| Le-Ann Harris, DNP, RN, NEA-BC | Director of Nursing, Critical Care & Trauma, | Increasing BSNs Work Group- Co-Chair-Practice |
| Jane F. Mahowald, MA, RN, ANEF | Executive Director, Ohio League for Nursing | Ohio Action Coalition, Nursing, Co-Lead |
| Maureen Sroczynski, DNP, RN | President/CEO | Consultant, Center to Champion Nursing |
| Cindy Wilkins, PhD, RN | Director & Chair of Nursing Programs, Muskingum University | Increasing BSNs Work Group- Co-Chair- Education |
Figure 2: Ohio Nurse Competency Model
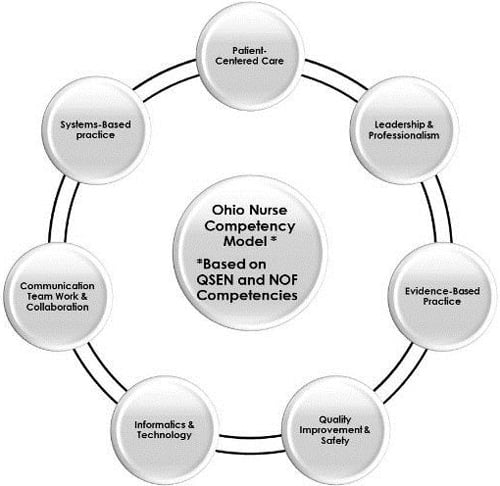
Table 2: Examples of Competency Statements for the Ohio Nurse Competency Model
| PATIENT-CENTERED CARE (QSEN) Definition: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient's preferences, values, and needs. | ||
| Knowledge Describe how diverse cultural, ethnic, and social backgrounds function as sources of patient, family, and community value. | Skills Provide patient-centered care with sensitivity and respect for the diversity of human experience. | Attitudes Seek learning opportunities with patients who represent all aspects of human diversity. |
| COMMUNICATION, TEAMWORK, & COLLABORATION (NOF-MA & QSEN) Definition: Interact, effectively, with patients and families and within nursing and inter-professional teams, to foster open communication, mutual respect, and shared decision-making, to achieve quality patient care and positive health outcomes, and to enhance patient satisfaction. | ||
| Knowledge Describe scopes of practice and roles of healthcare team members. Describe strategies for identifying and managing overlaps in team member roles and accountabilities. Recognize contributions of other individuals and groups in helping patient/family achieve health goals. | Skills Function competently within own scope of practice as a member of the healthcare team. Assume role of team member or leader based on the situation. Initiate requests for help when appropriate to situation. Clarify roles and accountabilities under conditions of potential overlap in team member functioning. | Attitudes Value the perspectives and expertise of all health team members. Respect the centrality of the patient/family as core members of any healthcare team. Respect the unique attributes that members bring to a team, including variations in professional orientations and accountabilities. |
May 26, 2017
DOI: 10.3912/OJIN.Vol22No02PPT37
https://doi.org/10.3912/OJIN.Vol22No02PPT37
Citation: Carissimi, K., Burger, J., (May 26, 2017) "Bridging the Gap: Seamless RN to BSN Degree Transitions" OJIN: The Online Journal of Issues in Nursing Vol. 22, No. 2.
yoderafteptelle1936.blogspot.com
Source: https://ojin.nursingworld.org/table-of-contents/volume-22-2017/number-2-may-2017/articles-on-previously-published-topics/rn-to-bsn-degree-transitions/
0 Response to "Continue Pathways Toward Increasing the Percentage of Nurses With a Baccalaureate Degree"
Post a Comment